Internal Family Systems (IFS) therapy is a relatively recent therapeutic approach developed by Richard Schwartz. It describes the psyche as having multiple parts with a centralized Self—or, your core essence. Within the Self are Parts, each with its own unique characteristics, emotions, and motivations. These Parts can be in conflict with each other, leading to inner turmoil and psychological distress.
Dr. Schwartz created IFS to identify Parts of the self1 and change how those Parts interact; it’s used in interpersonal psychotherapy and in group settings. Healing damaged Parts and addressing self-protectors can identify trauma, legacy burdens, and deep pains. Then, the client and therapist work together to soothe the Parts and create a sense of safety that allows clients to heal their parts on their own.
IFS and other forms of therapy can also address deep-seeded legacy burdens, which are conscious or subconscious burdens from generational trauma, family legacies, and family expectations that affect your life.
What Is Internal Family Systems Therapy (IFS)?
IFS therapy offers a comprehensive framework for understanding and addressing the complexities of the human psyche, both at an individual and systemic level.
IFS is based on the idea that each person’s mind is made of “Parts”2 that form around a traumatic experience. The Parts compensate for trauma and strive to protect Exiles, which are the isolated Parts carrying hurt and trauma.
Managers and Firefighters, the other 2 Parts, both work to keep Exiles hidden and safe.
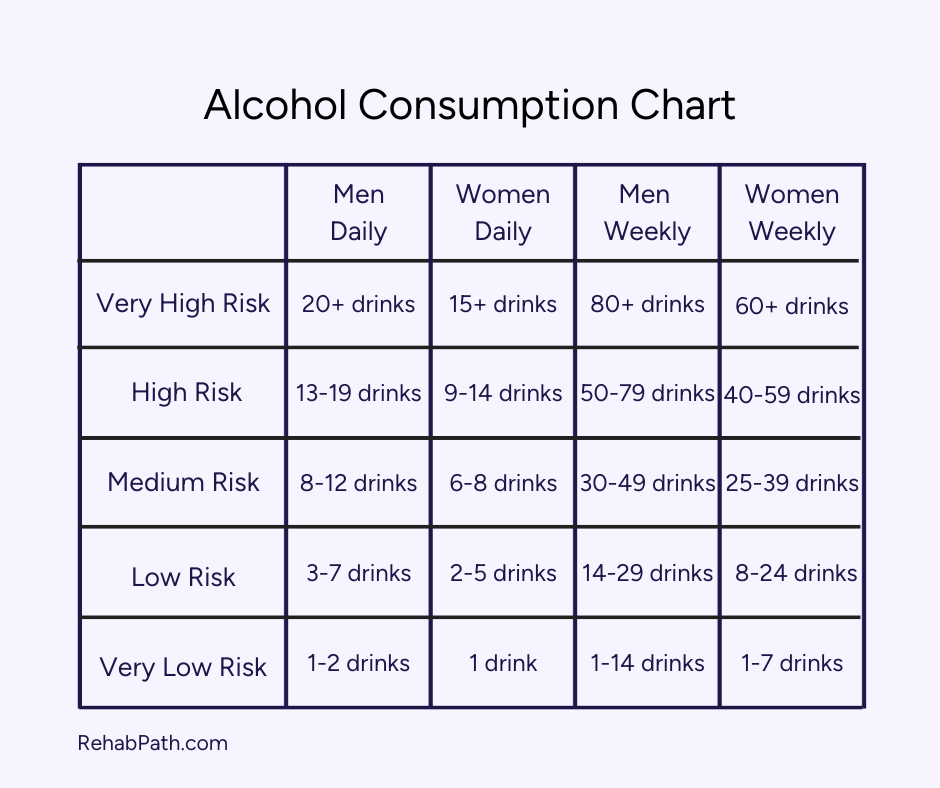
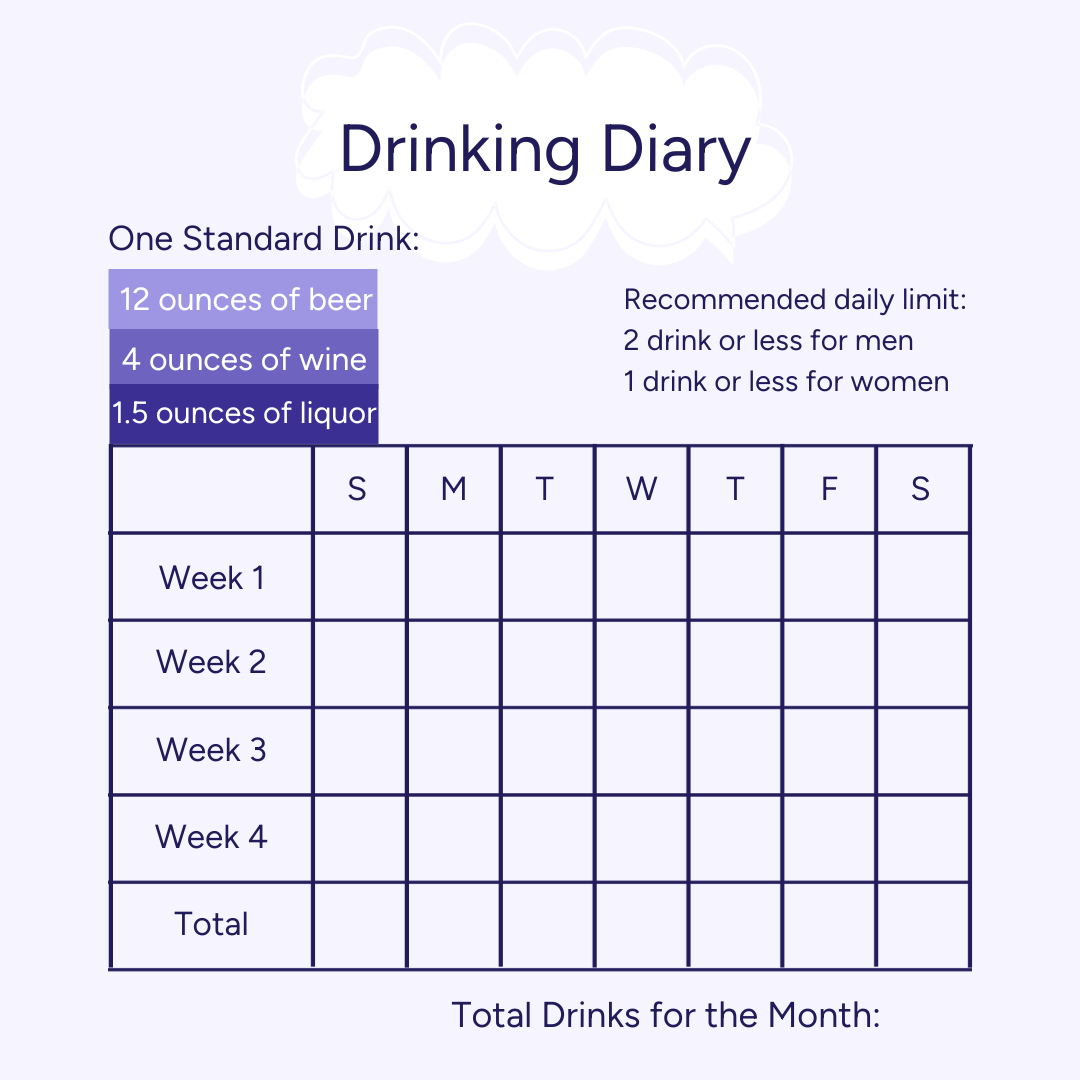
Your Firefighter Part is responsible for behaviors like drinking, drug use, and self-harm. These behaviors arise to control the Exiles’ feelings (terror, rage, grief, fear). Manager Parts find control through carefully evaluating situations, caretaking, and controlling. By staying in control, Managers think they can protect you from further pain and rejection.
Healing The Parts in IFS
In IFS, you’ll learn to hold space for the vulnerable Parts and meet them with compassion, a core part of the Self. IFS therapy helps you create a safe internal environment to confront your protective and vulnerable Parts and engage your compassionate Self. This safe internal environment can help you process traumatic memories and release legacy burdens without retraumatization.
IFS also connects your mind and body to increase mindfulness. You’ll become more aware of what you’re feeling and why, and where it may hold itself in your body.
Ultimately, IFS draws on “the inherent wisdom of the Self2” to rework cognitive distortions from childhood trauma, legacy burdens, and negative views of self. It’s done compassionately and without judgment, allowing the Parts to accept healing and back away from their maladaptive coping strategies.
Therapists are trained to provide IFS therapy. Not all therapists will offer IFS, and some will be more experienced than others. Check with your provider to see if they’re trained in IFS and their level of experience.
IFS for Trauma and PTSD
IFS can help those with trauma and PTSD become “compassionate witnesses”2 to their traumatic experiences without feeling overwhelmed or retraumatized. Patients use mindfulness to separate from the emotions, sensations, and images of their trauma. That mindful separation can strengthen their ability to reflect on their experiences as caring, compassionate observers.
For example, a patient may have residual shame after childhood abuse. IFS would help them step away from the shame, address the Part responsible for it, and allow their Self to replace the shame with self-compassion. Releasing the shame and allowing self-compassion can then reduce the hold of the traumatic experience and help the patient step into the present (and feel safe doing it).
Legacy Burdens: What They Are and Their Effects
A legacy burden leaves an imprint on future generations’ worldview and wellness. It can stem from one person or exist across a generation of people groups as generational trauma.
A single-person legacy burden could be caused by a belief carried down. For example, one of your grandparents or a parent may impose a belief on you and others in your family. The belief could be that you need to earn a lot of money, stay in a particular religion, or have a specific relationship. Even if you don’t necessarily believe their beliefs, the internal burden of their beliefs and expectations can still affect you.
Generational Trauma and Legacy Burdens
Generational trauma also leaves a legacy burden3. Indigenous and marginalized groups often carry trauma from generations of gentrification, colonialism, and brutality.
Stress and trauma can pass between generations through genetic changes3. Environmental stress can molecularly affect how a parent’s genes function, which then pass down to their child. Parents may also recreate their trauma and traumatize their children in turn. Generational trauma can pass down through a combination of the 2 as well.
The generations who didn’t experience the trauma firsthand may still experience the residual effects through their parents. Distant parenting, witnessing parents suffer from trauma, and avoiding the topic can strain relationships and create unhealthy attachment patterns. Some also feel the need to hold onto the trauma to honor those who directly went through it and bring awareness.
Interestingly, positive change commonly occurs in the third generation3. Grandparents, for example, may be more willing to share their experience with their grandchildren. It could be because enough time has passed, and because the third generation is more likely to seek growth and healing. This, in turn, can help the first and second generations heal.
Generational trauma can also create resiliency. Some children may see the burden carried in their lineage and actively pursue healing for themselves and others—which can turn into a sort of legacy burden itself. But, having a legacy burden doesn’t automatically entail generations of suffering. Individuals and groups can end the cycle, sometimes through IFS therapy.
IFS as a Healing Tool for Legacy Burdens
IFS can address the Parts carrying legacy burdens, allowing the Self to heal and prevent the trauma from extending. For some, their Exile may need healing. Others may need to heal a Firefighter or Manager to learn new coping tools.
Once the Part with the legacy burden feels safe and heard, the Self can bring in compassion and perspective, allowing you to detach from the burden. Continued IFS sessions and homework from your IFS therapist can help you maintain this release and continue forward.
Your legacy burden may surprise you once you identify it, or it could be an obvious burden carried through your family (like alcoholism or racism). In either case, IFS and other therapies can help you identify the burden and use your natural capabilities to heal.